Earning Employee Satisfaction Is a Process
Transcend’s recent national workforce research offers several important insights into where providers can strengthen their recruitment and retention. One of the major themes we saw come through was how critical process improvements and clarity of communication are to increasing the job satisfaction of senior care workers. In fact, the nursing workforce considers these areas second only to pay in importance to their overall satisfaction with their employer. And both of these factors show the greatest satisfaction gap between what respondents found important and how satisfied they are with those aspects in their current job.
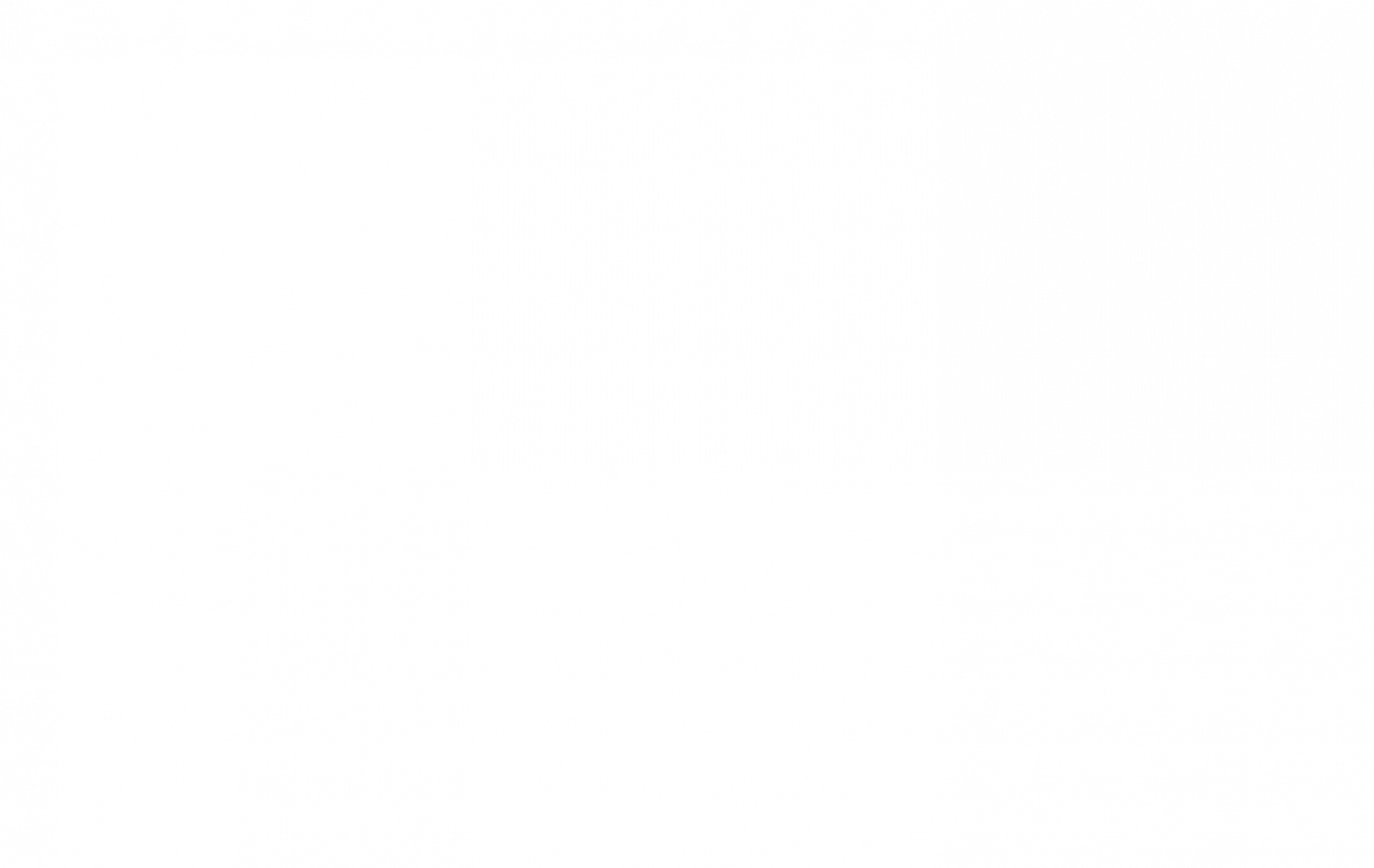
It might seem surprising that process and tools would rank so highly in importance to employees, higher than areas like work-life balance, a sense of purpose, culture or quality time with patients. In analyzing the research results, and seeking to answer why the nursing workforce answered the way they did, we found that a Maslow-inspired hierarchy of needs was a helpful way to frame up their priorities.
At the peak of this hierarchy are ultimate fulfillment in one’s career and a strong sense of purpose and passion. Transcend data (and experience) shows the nursing workforce is more likely than the average U.S. worker to value work beyond income and be in the field because they are seeking that sense of fulfillment. However, just as with the original Maslow hierarchy of needs, an individual’s focus will primarily be on the lowest need they don’t feel is being satisfied. The summit must be built up to, and our research shows there are barriers along the way.
Obviously, if one doesn’t feel they can put food on the table or pay their mortgage, or is not assured that they are physically or psychologically safe, those will be their primary concerns until they are resolved (safety concerns are another major challenge our research shows home care faces). Likewise, if they are bogged down with the tedium and confusion that results from poor process and communication, that will preoccupy them and leave less energy to dedicate to the quality care and patient connections that got them into the business to begin with.
Empower Employees to Work in Meaningful Ways
Focusing on effective processes and communication strategies – along with examining other factors like flexibility and workloads – will help your employees stay focused on what matters during work hours, while enjoying the time, freedom and resources to tend to the rest of life. These critical factors heavily influence the real daily lived experience of your team, part of the reason why improvements here can dramatically impact their overall satisfaction with their job.
Another reason this is so important: It’s likely that the staff who get the most frustrated with inadequacies in process and similar areas are your higher-performing employees – the kind not content to clock in and out but who want to see the results and feel like they’ve made a meaningful impact. They are the most likely to become discouraged when their organization doesn’t help or gets in the way of those aspirations. We’ve seen this exact trend play out in recent work with clients.
As noted earlier, compensation and process were the top two satisfaction gaps for employees. When we later asked respondents who said they were imminently considering leaving their current employer why they wanted a change, the top two responses were inadequate pay and burnout. There seems to be a link here, suggesting improvements to process, efficiency and communication/clarity can also play a big role in mitigating some of the key causes of burnout, the greatest turnover threat (45% of RNs who want another job say it’s because of burnout).
What to Do?
Your nursing workforce wants to focus on their calling, their passion for caring for others. However, employers must help remove barriers to that focus. For instance, time management and communication training, process refinements or electronic tools that reduce the time nurses must deal with the tedium of charting or inefficient team communication means more face time with patients (which is, unsurprisingly, considered very important to job satisfaction by those in home care).
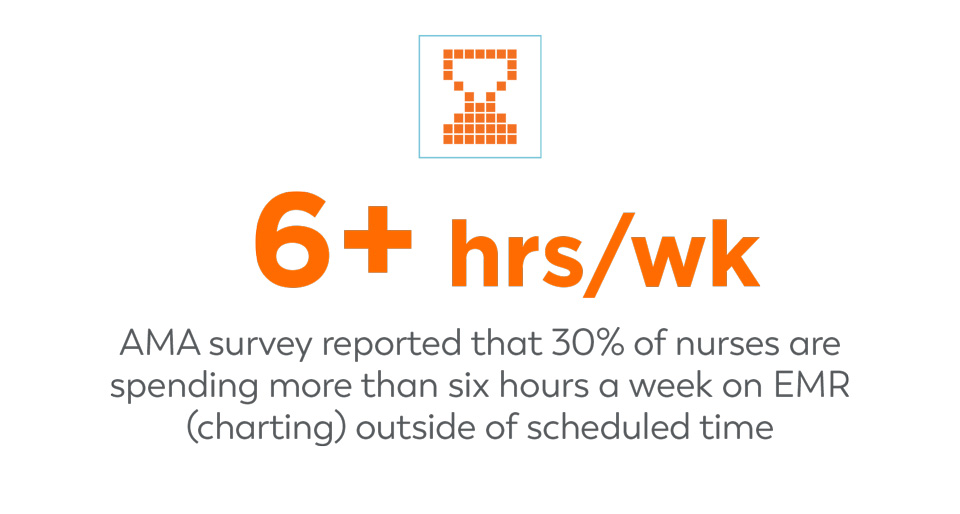
We know charting is the bane of existence for many nurses. And many cited this specifically and unprompted in our research. It is probably one of the most significant factors pulling the nursing workforce away from the part of the job that engages them, and robbing them of their personal time as well. In fact, an AMA survey reported that 30% of nurses are spending more than six hours a week on EMR (charting) outside of scheduled time – almost an entire workday of unscheduled work. While not all nurses love the idea, one partial solution is encouraging them to do charting while with the patient – to whatever degree it’s possible. Additionally, we’ve seen providers find success with establishing designated working hours for charting to minimize or eliminate the amount of it staff must do during after-hours.
Stepping back a little further, the key to strong process starts with strong leadership – and your middle management can play a significant role. When healthcare workers were asked what they wished their leadership/managers better understood, the most common responses were ones saying they felt like their managers did not truly grasp the work they were doing or that they were out of touch with the day-to-day realities of the job. Many said they wish their managers would get in with their team more often to more clearly understand these daily aspects so they would be better equipped to meaningfully support them – making decisions for the team that are well-grounded in their reality.
Management training that stresses leadership, culture building, communication and employee empowerment – beyond meeting quality and other metrics alone – can support that dynamic. Additionally, ask nursing managers when they last did a ride-along with their staff. Often, we see that leadership are RNs who don’t realize how much the field has changed since they were in that role. To encourage this kind of ongoing interaction, here are some questions your management team can use to check in with their reports:
- What are the biggest pain points for process they are experiencing?
- What is taking longer than it should?
- What are the most common frustrations in team communication?
- Where is clarity lacking the most?
- How long does charting usually take them? How much are they doing it outside of work hours?
- What time management strategies are they using – what’s working, what isn’t? (Also: Consider if additional training on time management skills would be helpful for your workforce)
- Can technology such as telehealth tools help make their workday more efficient? If so, what tools do they think would be most helpful?
With your leadership and process tuned into the needs of your workforce, you free your employees to focus more on the fulfillment they find in their role. Improvements here will also make efforts you put into building your organizational purpose, vision, culture and brand far more effective – as employees will be in a space where they are receptive to seeing how their individual passion ties into organizational goals.
For more workforce insights, be sure to check out our in-depth e-book on the national study results.