Navigating the COVID shift of caregiver minds
![]()
By Dave Hochanadel & Stan Massey
COVID-19 has completely changed family caregivers’ perspectives.
What are the long-term implications for senior care?
The COVID-19 pandemic has accelerated the arrival of an inflection point in senior care. One that, among other effects, has dramatically shifted the attitudes and expectations of family healthcare decision makers and will continue to impact their choices well beyond the current crisis. Taking action now is critical to setting the foundation for surviving and thriving during and after the current storm.
To help guide you on the path to sustainable growth in the challenging months and years ahead, Transcend Strategy Group has invested into new research on the attitudes of these family care decision makers. Our national survey revealed a range of new expectations related to safety, quality, services and communication, many of which will become part of the fabric of tomorrow’s normal. This spells accelerated opportunities for services that were already rife with potential, such as telehealth, while posing new challenges across the board to many aspects of culture, communications and operations.
Here we will explore the specific insights uncovered, the long-term implications and the actions you can take to adapt your organization to meet future demand. Ones that will help you increase census, improve retention, strengthen culture and deepen relationships with referral sources.

of respondents said COVID-19 completely changed their opinions about the best way to care for aging seniors.
For good and for bad, one thing is certain: Family care decision maker’s long-term perspectives on senior care have dramatically shifted in light of the pandemic.
In-home and in-facility providers face both shared and disparate challenges
A strong preference emerged for expanded in-home care, fueled by the ongoing fear of infection, with many respondents not only indicating greater confidence in home care but also a desire to move their loved one back home even after the pandemic. However, regardless of whether respondents had a loved one in a facility or receiving in-home care, all expressed heightened concern for the well-being of both patient and caregiver.
Facilities and in-home providers are each experiencing their own host of challenges amid the crisis. For instance, many hospice providers struggle to gain access to patients, whether families are turning them away at a private residence or in a care facility.
Meanwhile, orders in many states limiting families’ ability to visit loved ones in facilities created or exacerbated rifts in communication and trust, as many families may have felt left out of the loop. However, the data was clear that facilities have a well-established level of trust from those with direct experience with them. Those with a loved one currently being cared for at a facility were the most likely to favorably rank their confidence and support of the quality facilities can provide.
Perceptions have dramatically changed, with preference shifting to the home.


quality care can be provided in the home
to choose in-home care services

quality care can be provided in facility
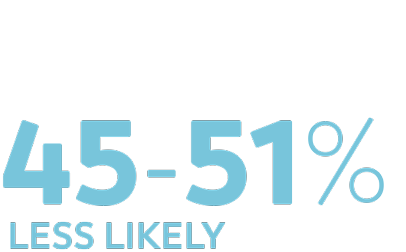
or “definitely won’t use” in-facility care
Whether in-home or in-facility, most families are worried about the safety of both their loved one and caregivers.


about their loved one being exposed to the virus by a caregiver

for the safety of the caregivers visiting homes

about their loved one catching COVID-19 at the facility
plan to use in-home care as a substitute for in-facility care even after the pandemic.
While overall trust in facilities suffered, those with a loved one already in a facility’s care generally viewed them favorably.

Families with a loved one already living at a facility are generally satisfied with the response to COVID-19.
44% of respondents had planned but postponed the following care for a loved one
Home healthcare |
14% |
||
Physical therapy or rehabilitation services at home (as an outpatient) |
12% |
||
At-home companion care |
12% |
||
Assisted living (at a facility) |
9% |
||
Physical therapy or rehabilitation services at an inpatient center |
9% |
||
Long-term, inpatient skilled nursing care at a facility |
6% |
||
At-home skilled nursing care (or private-duty nursing care) |
6% |
||
At-home palliative care |
5% |
||
Palliative care at a facility |
4% |
||
Hospice care at home |
3% |
||
Hospice care at a facility |
2% |
||
No, none of the above |
56% |
Three dimensions to focus on
COVID-19 sparked a long-term challenge. Even when the pandemic is over, the ripple effect of families’ perceptions and expectations of senior care providers will continue far into the future.
This is a marathon, not a sprint, and it will involve addressing three essential overarching needs for families and patients:




Trust needs to be continually reinforced, or in some cases re-established in the relationship between families and providers. Families need to be reassured providers are doing everything they can to take care of their loved ones during and eventually in the aftermath of the pandemic, and they must continually see how words are aligned to actions.
Providers need to make sure they understand the family’s needs and wishes, manage expectations and perform as promised. The trust built must be reinforced at every step of the patient experience; each one is an opportunity to strengthen or damage it.
“Emotional experiences are essential to create change. All of them are moments of interaction with our brand, and we must be mindful of them.”
Kristen Yntema, President & CEO, AuthoraCare Collective

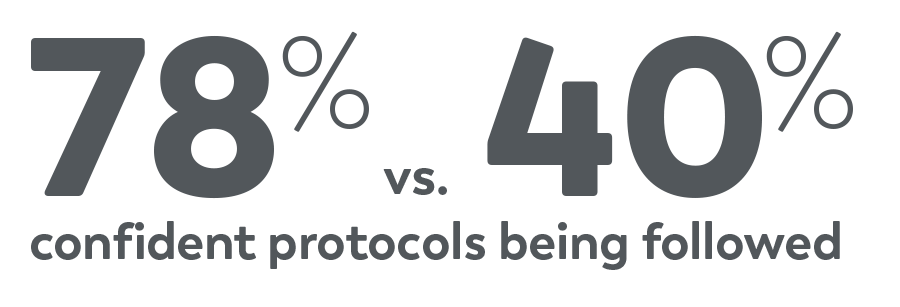
Many families already believe providers are delivering quality care and following necessary protocols. However, healthcare professionals must still reinforce their team’s expertise and explain specifically what they’re doing to minimize the risk of COVID exposure.
Maintaining a message about the quality and credibility of a provider’s capabilities, their years of experience and skilled interdisciplinary team will be critical to keeping families, patients and referrers alike confident. Further, families are hungry for credible information amid all the uncertainty, and providers have a prime opportunity to become a reliable resource for them.
There’s a disconnect between the data and reality. It’s because of passive communication. It’s clear we have the opportunity to be more intentional and to lead the conversations more proactively.
Lisa Novak, CEO, Northern Illinois Hospice

With their loved ones being among the most vulnerable population to COVID-19, compounded by factors such as limited or no access to facilities, the pandemic has left many families feeling powerless. They crave a reassuring sense of safety and security, which extends into desire to feel in control of the situation so they can best protect their loved one. It’s time to go the extra mile in keeping patients and families involved in making decisions; making sure to clearly understand their needs and wishes; and honoring their preferences on how and, for in-home patients, when care is implemented.
Additionally, ongoing and long-term policies, protocols and practices to stop the spread of infectious disease should be implemented, made highly visible and communicated to families (and referrers).
Paving the path forward
Addressing each of these three areas must involve efforts across an organization’s communications, culture and operations – creating a unified approach across what is outwardly communicated, internally believed and routinely implemented through procedures and protocols.
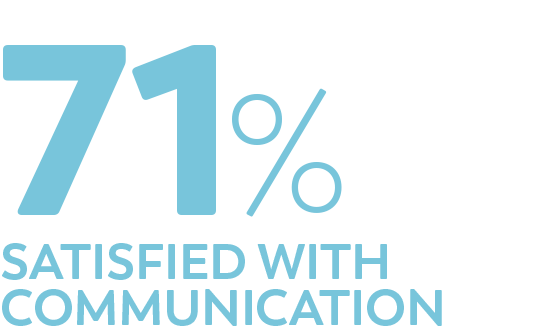
Better communication equals better perceived care
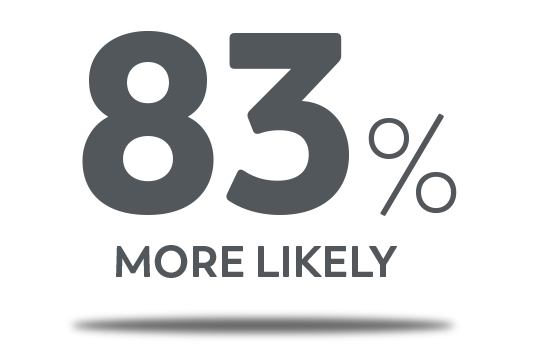
What came through loud and clear from the research was just how critically linked the quality of communication is with decision makers’ perception of the overall quality of care. Respondents were two or three times more likely to rank providers more favorably in metrics of care quality when they felt satisfied with the level of communication, clarity and honesty they are receiving from the provider. In fact, this was one of the greatest statistical correlations noted out of the research, and the correlation was greatest for facility-based providers.
As providers put new procedures and practices in place, communicating frequently and consistently is vital. It will remain increasingly important to focus on elevating patient, family, prospect and referrer communications – keeping all parties informed and showcasing what is being done to address COVID-19 or other infection control related needs in the future.
Now is also the time to make sure you have a strong internal communication platform. Keep your staff up to date on all aspects of patient care, challenges and opportunities. Constantly seek their feedback on how to further improve. Develop an employee value proposition and communicate consistently against it. Educate and train your team to reinforce the trust, credibility and control families are craving.

Respondents nearly twice as likely to be confident in quality of in-home care if they’re confident they’ll receive open, honest communication.

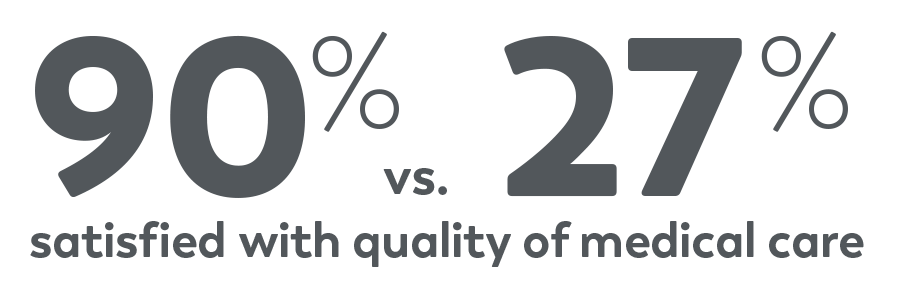
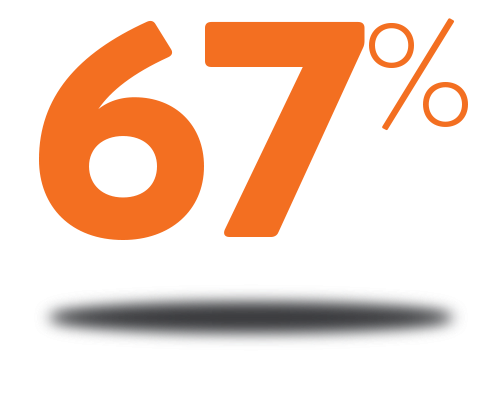
Respondents more than three times as likely to be confident in quality of in-facility care if they’re also happy with the quality of communication received about COVID-19 cases.
Families expect facilities to have a system in place to better communicate in the event of future crises.

Evolve your messaging
Those who thrive will have a clearly defined brand and purpose, and effectively live that purpose through everyday actions. Rather than focusing messaging on feel-good communications (of which there are already countless trite examples), such as with a vague commitment to “being there for you,” focus on providing useful information and tangible solutions to the concerns your audiences are facing.
Demonstrate to current families and prospects how you’re living your brand and purpose to provide quality care, quality communications and the best overall patient experience while keeping patients as safe as possible. Communicating safety protocols and care plans consistently, frequently and through the language of your brand will show how the actions you are taking reflect your passion and mission – continually reinforcing your credibility.

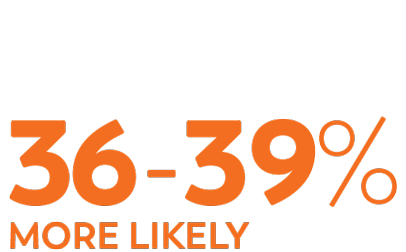
to now believe quality care can be provided in a home compared to a facility

out of those who receive in-home services
In order to capture those who are more open than ever to in-home care, now is the time for in-home providers to educate families on both the advantages of keeping patients at home where they might prefer to be, as well as showing why your team specifically should be the ones providing that care. Additionally, what measures can you promise that you take on every visit to minimize COVID risks?

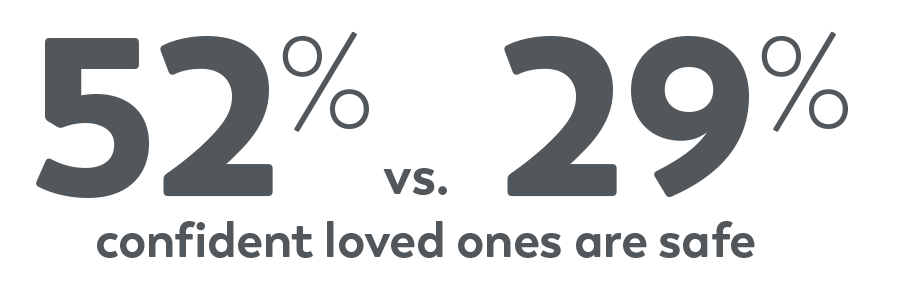
Respondents nearly twice as likely to believe resident is safer from viruses in a facility vs. in-home if they’re satisfied staff provides compassionate care when family can’t visit.
For facilities, since many residents or their families also choose a provider based on socialization and activities, it’s important to show how you have maintained this highly desired interaction safely for the best resident experiences possible. Showcase what you have done to help facilitate chats with family members, whether it’s virtually or via some of the through-the-window visits that have become a popular way to safely visit in-person.
Embrace the “digital front door”
Beyond exploring an evolution of your messaging, maintaining quality ongoing communication will also require re-examining the methods and media plans used. It’s especially important to reach audiences “where they are” during this COVID era.
As social distancing will be a part of our lives for some time still, your digital presence will play an even more critical role in reaching these audiences and creating a positive impression.
Now is a good time to evaluate your website, digital advertising and social media presence to make sure you are putting your best foot forward. Look at your entire digital presence in total, considering the experience from the vantage point of each key audience. What paths will they navigate through your digital ecosystem? Is it coherent and cohesive? Is the breadth and depth of information available suitable to substitute a loss of in-person contact?
Support families and patients with stronger and clearer resources, educational materials and tools they can use. Family caregivers in an in-home setting could especially benefit from your offering such support tools. It will demonstrate your care and compassion, while reminding them how much relief you can provide them.
Mind the entire service experience continuum
As the pandemic disrupts a number of traditional lines of communication, be sure to consider how you may compensate for that hinderance across all phases of your service experience continuum.
The experience begins when there’s a condition or disease trigger that precipitates the need for your care to begin with. Consider ways that tools such as your digital platforms can preemptively build awareness in these earlier stages for patients, families, referrers, payers and other audiences – so they are already primed to see you as a provider of outstanding care when the time comes for your services. On the other end of the continuum, seek alternative ways to maintain or strengthen relationships with families over the long term, who can become loyal advocates for your care to others.
Find new ways to engage referrers
One such way to build your presence in the awareness stage is to digitally bolster your outreach to referrers. Over the past several months, you may have seen your referral pipelines lighten or dry up completely. Now and into the future, it will be critical to find innovative new ways to deliver value to these sources. Taking these steps now can meaningfully deepen your relationships with them, sustainably increasing your referrals for the long term.
Efforts can include using social media channels, such as LinkedIn, to help keep top-of-mind, foster dialogue and reiterate all you are doing to keep patients safe. There are also new sophisticated advertising methods, such as account-based marketing (ABM), that can be used to reach key individuals within a referral source with laser focus on the messages they care the most about.
In-home providers can leverage Transcend’s consumer preference data to reinforce the point that most families are increasingly confident about in-home care. Package your clinical data to prove positive outcomes in terms that not only benefit the patient, but the interests of each referral source.
Develop an operations guide to deliver and demonstrate quality care
Putting practices and protocols in place to reinforce quality with consistency, and then readily communicating them, will play a major role in increasing confidence. A big part of this endeavor is in tangible practices to keep patients safer against the spread of infectious diseases like COVID-19.
Families’ shaken confidence will resonate after the pandemic passes. Formalizing or enhancing your operational approach to an infectious outbreak will show how you have learned from the events of 2020 and that it will ultimately serve to improve your long-term approach to keeping patients safer and happier.
Craft a telehealth strategy now, before someone does it for you
Telehealth not only can make more comprehensive and consistent care possible, it’s one tool that will play a major role in giving families and patients the sense of security and control they desire because they have a say in how/when they use it.
With families more receptive to it than ever and regulations making it easier to employ, telehealth certainly fits the bill of “an idea whose time has come.”

Telehealth provides an attractive opportunity and families say they’re more likely to use telehealth in the future.
As officials across the nation implemented social distancing requirements and stay-at-home orders, telehealth finally began to emerge as a critical asset for staying in touch with patients and families. Its growth was further aided by relaxed restrictions on the use of telehealth from CMS and many larger payers. HHS even began allowing providers to use platforms such as FaceTime and Zoom for virtual visits covering a wide range of conditions, from urgent care, primary care checkups, medication follow-up and COVID-19 screenings.
The time to begin building your long-range plan to further integrating telehealth technology is now. Doing so will help you position yourself as a leader guiding toward an outcome as opposed to being forced into it by referral partners or by families demanding it.
Keep in mind that telehealth can include much more than video chats, as detailed on our blog. Also, remember that telehealth not only empowers efficient provider-to-patient/family communications (for regular check-ins, remote assessments, caregiver training and support) but also provider-to-provider contact (for remote IDT meetings, staff check-ins and consultations with other treating clinicians).
The future is the experience-centric model
As has been the case more broadly in healthcare, COVID-19 has further accelerated preference for an even more consumer- or experience-centric model. A shift further spurred along financially by changes in reimbursement models, with the increasing influence of satisfaction scoring.
Putting patients and their families in control – giving them a sense of increased security, continually gaining their trust through regular and concrete communication and relentlessly building your credibility – will be cornerstones to growing sustainably in our post-COVID reality.
What research do you want us to explore next?
Discover how you can participate in defining future research initiatives that yield insights that help your agency grow. Contact Stephanie Johnston to learn about how you can join the new Transcend Research Consortium.
Appendix: About the research
Survey Respondents
1,000 Family Healthcare Decision Makers
ages 40 to 65
40 to 49 – 23% 50 to 59 – 55% 60 to 65 – 22%
In-home use among respondents |
|||
|---|---|---|---|
Home healthcare services |
24% |
||
At-home physical therapy or rehabilitation |
21% |
||
At-home skilled nursing care (or private duty nursing care) |
18% |
||
At-home companion care |
16% |
||
At-home palliative care |
7% |
||
Hospice care at home |
4% |
||
No, none of the above |
49% |
In-facility use among respondents |
|||
|---|---|---|---|
Assisted living community |
23% |
||
Skilled nursing center |
13% |
||
Hospice care center |
5% |
||
No, none of the above |
66% |