Building a true patient-centered brand
![]()
By Dave Hochanadel & Stan Massey

As competition continues to heat up for the same pool of prospective patients and staff in any given community, providers of home-based healthcare must find more potent ways to differentiate themselves in their respective markets.
For most, part of that formula for success includes building a distinctive “brand.” “Brand,” however, might be the most overused marketing term there is. And one of the most ambiguously understood. Today, it is most commonly seen as the “essence” or DNA of an organization – the personality, mission statement, value proposition and underlying “why” that drives the brand identity – and the outward communication of these aspects. This is all true, but nowhere near the whole truth.
You can have a carefully crafted mission, differentiated look and voice, and impeccable advertising and marketing platform that set you apart from others in your region. But someone’s perception of your home health or hospice agency can all fall apart after one negative interaction with a real live person.
Brand is better defined as the culmination of every interaction someone has with an organization, or with any of their products or services, which directly impacts their perception of the experience and satisfaction.
This is why the best patient experiences depend upon a strong brand, one that is driven by an ecosystem where culture (blending identity, purpose and mindset), operations and communications all work in sync throughout a patient’s journey.
Culture, operations and communications must work in sync throughout a patient’s journey.
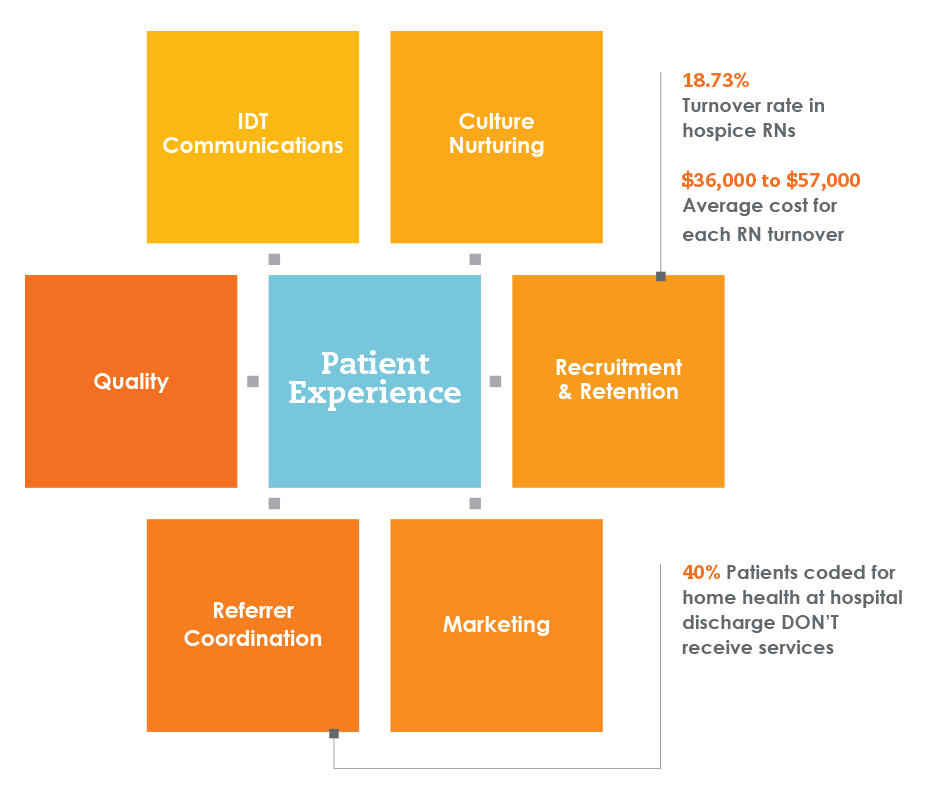
Focus areas to connect your team to the best patient-centered care
When building a culture of excellence, language matters.
Home Health Compare rates a national average of 83% for the overall care score patients give their agency. Closing that gap from acceptable to exceptional requires culture and operations that reflect your brand so powerfully that it is expressed in every interaction and through every team member. Creating this consistency relies heavily on a culture that is working from the same playbook – and speaking the same language.
The way a culture communicates, thinks and acts continually influence each other. Building exceptional patient experiences depends upon creating a system that supports a consistent patient-centric POV across all three. When one falls out of alignment, the others follow.
And if you think you’re already hitting all of these points, your patients might disagree.
Plain talk vs. clinical speak.
Every home health and hospice agency Transcend Strategy Group has worked with over the past 20 years shares the core value of wanting the patient and family to have exceptional experiences. Our careful examination, however, has revealed how easy it can be to falter from that intended mission in day-to-day conversations and actions. The culprit? Often, it starts with the language. It can often slip into “clinical mode” – causing the mindset, unintentionally, to shift back from the patients’ to the clinicians’. For instance, an agency may discuss with a patient a goal of being able to walk 200 feet without fatigue. But what if we took a moment to investigate more deeply what the most meaningful goals to the patient are, in their terms? It could be reading a book to their grandchild without getting short of breath. Or simply walking down their driveway to get the mail.
Patients and families associate hospice with imminent death in a matter of days and say they or their loved one “isn’t ready for hospice.” But when the conversation is open-ended and empowers patients to share their goals, they often start describing the benefits and attributes of hospice care. “I want to stay in my own home … I want to keep my pain under control, but not drugged out of my mind … I want to see my grandson graduate from college next month …” By confirming that those types of goals are exactly what hospice care supports, patients and families often become much more receptive.

When organizations start by talking with patients about their goals, it opens up their willingness to accept services more readily.
These language barriers often begin with the terminology of the services themselves. For instance, Transcend’s proprietary surveys conducted with thousands of family healthcare decision makers show only 30 to 35% had even heard the term “palliative care” before, and only about 10% could define it. Yet, many providers launch right into discussing palliative care options. As with any specialization, it’s easy to forget that the terms we take for granted can be a foreign language to those not in it every day. Taking the time to explain the benefits of palliative care are much more relatable to patients and families than the label we’ve put on the service.
Other misperceptions exist about home health. For instance, Medicare data shows that about 40% of patients coded for home health at discharge from an inpatient hospital stay don’t receive home health.
Part of that is their misperception that home health is just help with activities of daily living around the house, not the expert clinical and therapeutic care that it really is.
Strong culture, reinforced by operational excellence, can sustain a patient-centric mindset across the organization and through daily actions – one that reinforces the importance of defining and discussing every aspect of care in a way that is deeply connected to the patient’s perspective, not the clinician’s.
When the conversation is changed internally, it inevitably reshapes the ones happening with patients. The patient will likely better understand benefits of their care and can help them work with care providers to define goals that are the most meaningful to them. This ultimately improves their perception of and satisfaction with the care they receive.
Culture and operations that empower your team to consistently work with clarity, purpose and passion are what will ultimately influence the nitty gritty, daily interactions that they have with patients. Those are the ones that will impact your patients’ experience most of all.

of healthcare decision makers couldn’t define the term “palliative care.”
How are you measuring the impact of patient experience?
A couple of popular sayings are relevant to this discussion:
“What matters gets measured” and “What’s measured gets managed.”
So, how are you measuring and managing the impact of your culture, operations and communications regarding the patient experience? Are you using a QAPI approach for quality assurance and performance improvement? Do you proactively seek to improve CAHPS or HHCAHPS scores? Are you scrutinizing OASIS assessments to identify quantifiable areas for improvement?
Engrained in these quality measurement programs is the importance, once again, of language and communicating in a consistent way to drive improvements. For example, CAHPS surveys and Hospice Compare
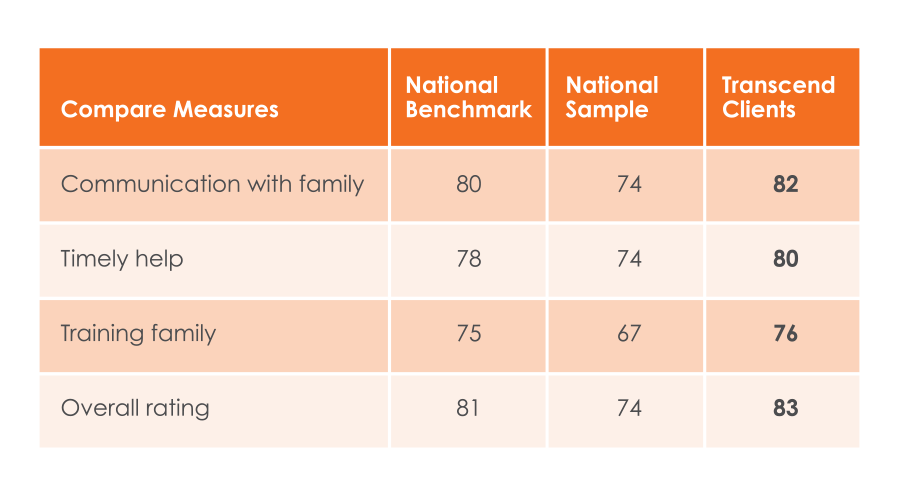
reports are purportedly objective measurement tools because families served by any hospice are asked the same set of consistent questions for apples-to-apples evaluations. However, when you look at the language of the questions and reports, terminology can have very subjective leanings.
Hospice Compare categories include “Getting timely help” and “Treating patient with respect.” What does “timely” mean to any given family? How does each individual family define “respect”? How do you make sure your team is consistently communicating these qualities in ways that are meaningful to patients and families?
Home-based healthcare providers could benefit from similar tools and disciplines of quality measurement and improvement from the manufacturing sector. Transcend Strategy Group can offer guidance and insights in this area if you are interested in exploring the possibilities further.
Great culture brings great talent.
Strong culture and operations with measurable quality not only improve the patient experience, it enhances your staff’s as well – benefiting both recruiting and retention.
Engaged employees give more effort and are more likely to embody your brand’s values.
Supported by the right system, language and tools, a patient-centric brand becomes self-perpetuating – attracting the best, most passionate talent who want to work somewhere that expresses a shared viewpoint. A powerful cycle that continues to inspire and invigorate staff’s innate desire for providing quality, compassionate care – what likely brought them to a career in healthcare to begin with.
A study by Dale Carnegie Training found that companies with engaged employees outperform companies without engaged employees by more than

Ready to rethink brand?
Transcend Strategy Group can help. We combine branding expertise with intimate knowledge in how the home-based care space works to ensure your principles come to life through every employee and for every patient.