Three Keys to Building a Viable Palliative Care Program (Part 2)
Does your agency currently run a home-based palliative care program? If so, are you struggling to at least break even? Does a deficit prevent you from growing your program the way you want?
Or are you thinking about starting a palliative care program? Do you hear about the challenges other providers are having and they give you pause? Are you wondering about or exploring the best way to begin?
For Transcend’s latest podcast episode, I interviewed Mark Hendrix, president of nTakt – a company focused on building sustainable palliative care programs – and Amanda Copeland, AGNP, an experienced palliative care nurse practitioner who is still providing hands-on care in the field.
You can hear our conversation through the podcast link below. In fact, this discussion is the second of a two-part series featuring Mark. If you haven’t listened to Part 1 yet, you can listen here.
In addition to the sound advice Mark and Amanda give, the Center to Advance Palliative Care (CAPC) and the Palliative Care Quality Collaborative (PCQC) recently published a report that provides an interesting snapshot of home-based palliative care in our nation.
Combining information from Mark and Amanda with observations from the CAPC/PCQC report gives us three key considerations for building a sustainable palliative care program:
1. Think small. Mark and Amanda highly recommend starting a palliative care program on a smaller scale – including geography, staffing and patient volume. Mark says, “One of the key mistakes that I see is (providers) try to start a program and they put a lot of nurse practitioners all over a state in some cases, and none of those individual areas are efficient yet. Problems are just multiplied that way. So, start with a pilot program, start with a pilot area, get the processes down, get the billing down, fine tune it. And then expand.”
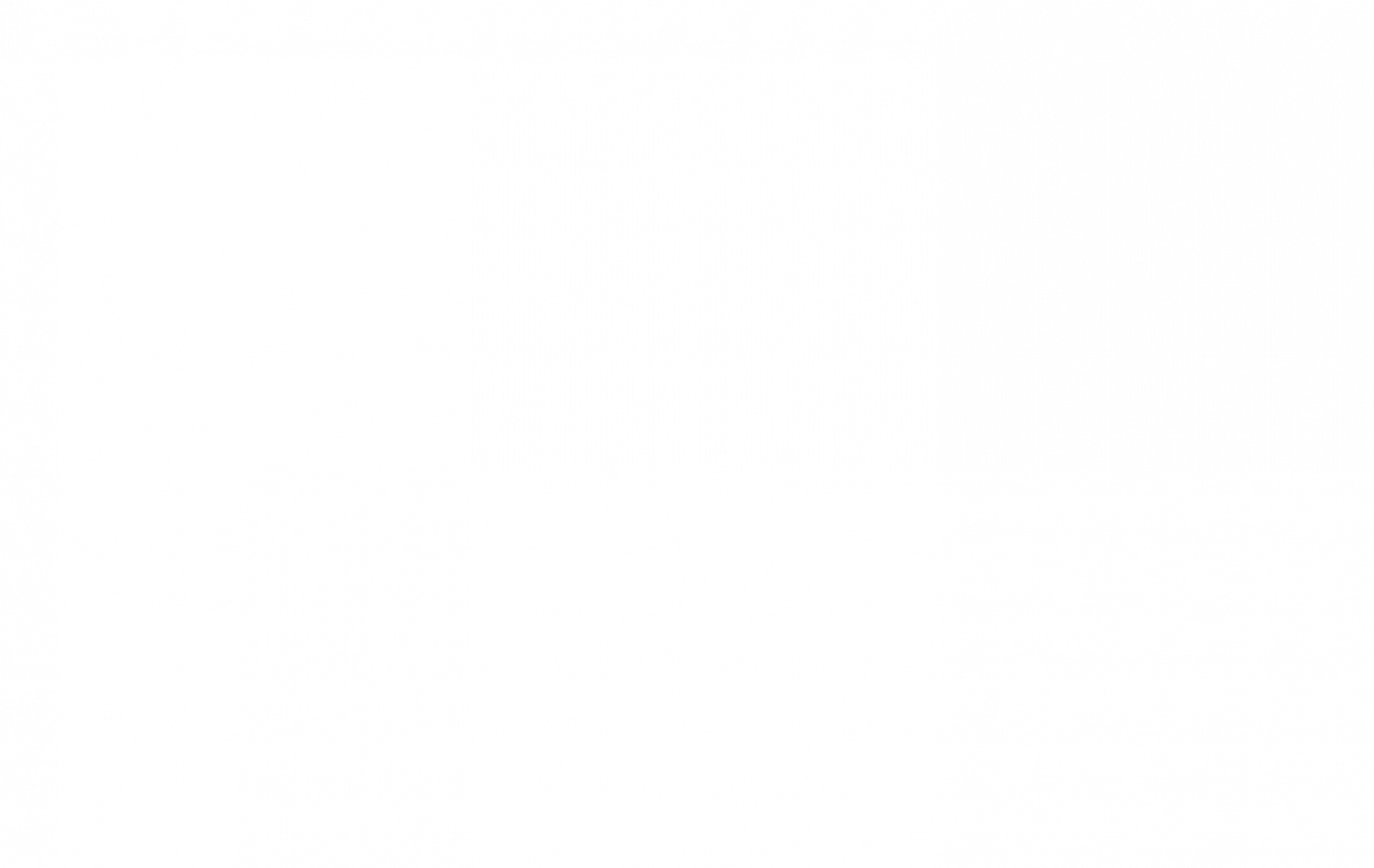
Statistics from the CAPC/PCQC report suggest the majority of programs are following this model of staying relatively small. According to their data, median patient volume is 205 patients served annually at home, with median ADC at 51.5 patients.
From a staffing standpoint, CAPC/PCQC reports palliative care programs on average maintain 5.8 full-time equivalent employees. The organizations also recommend that a program’s staff include at least three of the following positions:
- Physician (MD or DO)
- Advanced Practice Provider
- RN or LPN
- Social Worker
- Spiritual Care Professional
2. Maintain reasonable caseloads. Starting small works in conjunction with keeping caseloads manageable for the palliative care staff, empowering them to provide the highest quality care. Mark advocates for a nurse practitioner driven model, starting with four NPs on staff and one other key role, such as an RN or social worker.
Amanda suggests a model for managing caseloads for herself and other NPs on her team. She plans two-hour visits for new patients and one-hour visits for follow-up care – and schedules “equivalent” visits totaling four hours each workday (e.g., two new patients OR one new patient and two follow-ups OR four follow-ups).
The math works out well when also looking at CAPC/PCQC data. Their report says home-based palliative care practitioners spend an average of 41 minutes of roundtrip “windshield time” per patient. So if a practitioner has four follow-up visits, that’s an average drive time of nearly 2.75 hours each day. This total of patient visits and travel time accounts for about seven hours per day, leaving some time for charting or other duties.
Of course, the cadence of needs for different palliative care patients and a practitioner’s geographic territory can vary greatly. But Amanda says this model typically allows for each NP to effectively handle a caseload of 70 patients – enabling a patient census above the national median, even for a start-up.
You may have to adjust the formula for the specifics of your program, always keeping in mind the best interest of each patient and their family. Other solutions include the use of telehealth for some virtual follow-up visits that eliminate windshield time from the equation.
3. Partner with other providers in your community. Palliative care serves a vital role in the continuum of care – and it’s a role many providers avoid because of the financial challenges of operating a program that stays out of the red. So to perform palliative care well, Amanda and Mark emphasize that it’s important to stay focused on genuine palliative services. Amanda says, “You may get caught up in trying to do too many things that just prevent you from really staying focused on your palliative care role. I think the big part of that is just developing those relationships with other providers in the community, other providers that are a part of the team taking care of your patient, and having good communication and coordination of care with them to allow each of those to perform their role, whether it’s primary care or home health or the specialty of providers.”
Mark adds, “Palliative care shines in an environment where it provides a continuum between hospital, home health and hospice. It fills that gap that’s really vacant in our healthcare system today. I see a lot of programs that really get too much into primary care, or too much into other fields … such as DME, wound care, some of those type of things.”
In other words, palliative care programs should serve their exact role in the continuum of care, not try to BE the continuum of care. So, partnering effectively with other providers in your community will provide real value to your organization as well as theirs.
To that end, several of CAPC/PCQC’s recommendations underscore that – no matter how you decide to staff a palliative care program – your team should exhibit the traits that define genuine palliative care, including:
- Capability to conduct a comprehensive pain assessment
- Capability to create an effective care plan
- Proven competencies in pain and symptom management
Lastly, it’s crucial that your program curates data that proves positive patient-reported outcomes. Having the data that quantifies pain relief and other outcomes, such as reducing ER visits and hospitalizations, will be critical to attracting community partners and payers alike.
How will this information help you shape or improve your palliative care program? If you want an experienced partner in thinking through the business strategy of palliative care and how to promote your program to your community, Transcend stands ready to help. Email us anytime at hello@transcend-strategy.com.